Oculomotor nerve
The oculomotor nerve originates from the anterior aspect of the midbrain. It moves anteriorly, passing below the posterior cerebral artery, and above the superior cerebellar artery. The nerve pierces the dura mater and enters the lateral aspect of the cavernous sinus. Within the cavernous sinus, it receives sympathetic branches from the internal carotid plexus. These fibres do not combine with the oculomotor nerve – they merely travel within its sheath.
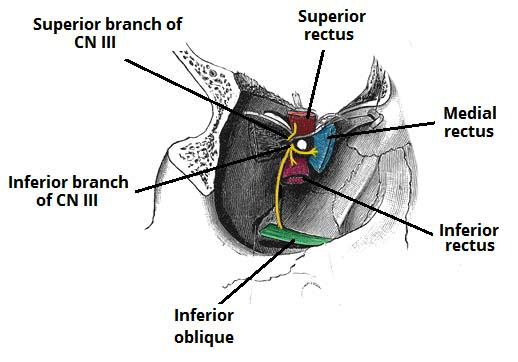
The nerve leaves the cranial cavity via the superior orbital fissure. At this point, it divides into superior and inferior branches. Once within the orbital cavity, both branches innervate accessory structures of the eye:
Superior branch: Motor innervation to the superior rectus and levator palpabrae superioris. Sympathetic fibres run with the superior branch to innervate the superior tarsal muscle.
Inferior branch: Motor innervation to the inferior rectus, medial rectus and inferior oblique. Parasympathetic fibres to the ciliary ganglion, which ultimately innervates the sphincter pupillae and ciliary muscles.
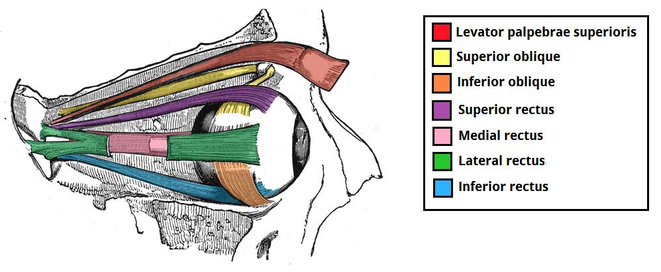
The oculomotor nerve innervates the majority of the extra-ocular muscles. These muscles move the eyeball and upper eyelid.
Superior branch:
- Superior rectus – Elevates the eyeball
- Levator palpabrae superioris – Raises the upper eyelid.
There are sympathetic fibres that run with the superior branch of the oculomotor nerve. They innervate the superior tarsal muscle, which acts to keep the eyelid elevated after the levator palpabrae superioris has raised it.
Inferior branch:
- Inferior rectus – Depresses the eyeball
- Medial rectus – Adducts the eyeball
- Inferior oblique – Elevates, abducts and laterally rotates the eyeball
There are two structures in the eye that receive parasympathetic innervation from the oculomotor nerve:
- Sphincter pupillae – Constricts the pupil, reducing the amount of light entering the eye.
- Ciliary muscles – Contracts, causes the lens to become more spherical, and thus more adapted to short range vision.
The parasympathetic fibres travel in the inferior branch of the oculomotor nerve. Within the orbit, they branch off and synapse in the ciliary ganglion. The fibres are carried from the ganglion to the eye via the short ciliary nerves.
Clinical relevance
Third cranial nerve disorders can impair ocular motility, pupillary function, or both. Symptoms and signs include diplopia, ptosis, and paresis of eye adduction and of upward and downward gaze. If the pupil is affected, it is dilated, and light reflexes are impaired. If the pupil is affected or patients are increasingly unresponsive, neuroimaging is done as soon as possible.
Third cranial (oculomotor) nerve disorders that cause palsies and affect the pupil commonly result from:
- Aneurysms (especially of the posterior communicating artery)
- Transtentorial brain herniation
Less commonly:
- meningitis affecting the brain stem (eg, TB meningitis)
The most common cause of palsies that spare the pupil, particularly partial palsies, is
ischemia of the 3rd cranial nerve (usually due to diabetes or hypertension) or of the midbrain. Occasionally, a posterior communicating artery aneurysm causes oculomotor palsy and spares the pupil.
The three main anatomical causes of an oculomotor nerve lesion:
- Increasing intracranial pressure – this compresses the nerve against the temporal bone.
- Aneurysm of the posterior cerebral artery.
- Cavernous sinus infection or trauma.
Note: there are other pathological causes of oculomotor nerve palsy such as diabetes, multiple sclerosis, myasthenia gravis and giant cell arteritis.