Common peroneal nerve
The nerve begins at the apex of the popliteal fossa, where the sciatic nerve bifurcates into the tibial and common fibular nerves.
The common fibular nerve follows the medial border of the biceps femoris, running in a lateral and inferior direction, over the lateral head of the gastrocnemius. At this point, the nerve gives rise to two cutaneous branches, which contribute to the innervation of the skin of the leg.
To enter the lateral compartment of the leg, the nerve wraps around the neck of the fibula, passing between the attachments of the fibularis longus muscle. Here, the common fibular nerve terminates by dividing into the superficial fibular and deep fibular nerves.
Click image to enlarge
The common fibular nerve innervates the short head of the biceps femoris muscle (part of the hamstring muscles, which flex at the knee)
In addition, its terminal branches also provide innervation to muscles:
- Superficial fibular nerve: Innervates the muscles of the lateral compartment of the leg; fibularis longus and brevis. These muscles act to evert the foot.
- Deep fibular nerve: Innervates the muscles of the anterior compartment of the leg; tibialis anterior, extensor digitorum longus and extensor hallucis longus. These muscles act to dorsiflex the foot, and extend the digits. It also innervates some intrinsic muscles of the foot.
If the common fibular nerve is damaged, the patient may lose the ability to dorsiflex and evert the foot, and extend the digits.

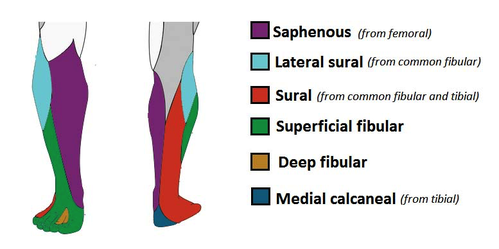
There are two cutaneous branches that arise directly from the common fibular nerve as it moves over the lateral head of the gastrocnemius.
- Sural communicating nerve: This nerve combines with a branch of the tibial nerve to form the sural nerve. The sural nerve innervates the skin over the lower posterolateral leg.
- Lateral sural cutaneous neve: Innervates the skin over the upper lateral leg.
In addition to these nerves, the terminal branches of the common fibular nerve also have a cutaneous function:
- Superficial fibular nerve: Innervates the skin of the anterolateral leg, and dorsum of the foot (except the skin between the first and second toes).
- Deep fibular nerve: Innervates the skin between the first and second toes.
Clinical relevance
Symptoms of peroneal nerve injury (foot drop) may include:
- Inability to dorsi flexi (point toes toward the body), evert the foot, or extend foot digits
- Pain
- Weakness
- Numbness (on the shin or top of the foot)
- High-stepping walk (called steppage gait or footdrop gait)
Common causes of damage to the peroneal nerve include the following:
- Trauma or injury to the knee
- Fracture of the fibula
- Entrapment neuropathie, e.g. use of a tight plaster cast (or other long-term constriction) of the lower leg, crossing the legs regularly, regularly wearing high boots, pressure to the knee from positions during deep sleep or coma, or injury during knee surgery or from being placed in an awkward position during anesthesia
The most subtle trauma that can cause denervation of the peroneal nerve is a closed deglovement injury, also known as a Morel-Lavallée lesion. Deglovement implies a shearing between the fascia and the subcutaneous tissues. This creates a potential space that fills up with serosanguinous fluid ranging from clear fluid to frank blood. A subcutaneous sensory branch passing through the fascia can be lacerated resulting in local hypoesthesia, as can happen to the superficial peroneal nerve in the lower third of the lateral compartment.
Intraneural ganglia are relatively rare compared to extraneural ganglia, but they should be considered in case of unexplained foot drop. Clinical and electromyographic findings are almost always more pronounced compared with extraneural ganglia, and this is related to the perineurium that restricts expansion of the intraneural ganglion and thus increases the pressure on the nerve.
Common peroneal nerve injury is often seen in people:
- Who are very thin (for example, from anorexia nervosa)
- Who have certain autoimmune conditions, such as polyarteritis nodosa
- Who have nerve damage from other medical problems, such as diabetes or alcohol use
- Who have Charcot-Marie-Tooth disease, an inherited disorder that affects all of the nerves
Electrophysiological tests are commonly performed, and they are an important aid in differentiating a peroneal neuropathy from a more proximal lesion or an L5 radiculopathy. There are several limitations to electrophysiological testing. It is hard to evaluate deeply located muscles, and these tests are relatively invasive, operator dependent, do not pick up denervation in the earliest phase and do not allow a complete evaluation of a muscle.