Ulnar nerve
The ulnar nerve is derived from the brachial plexus. It is a continuation of the medial cord, containing fibres from spinal roots C8 and T1. After arising from the brachial plexus, the ulnar nerve descends down the medial side of the upper arm. At the elbow, it passes posterior to the medial epicondyle of the humerus, entering the forearm. At the medial epicondyle, the nerve is easily palpable and vulnerable to injury.
In the forearm, the ulnar nerve pierces the two heads of the flexor carpi ulnaris, and travels alongside the ulna. Three branches arise in the forearm:
- Muscular branch: innervates some muscles in the anterior compartment of the forearm.
- Palmar cutaneous branch: innervates the skin of the medial half of the palm.
- Dorsal cutaneous branch: innervates the skin of the medial 1 and 1/2 fingers, and the associated palm area.
At the wrist, the ulnar nerve travels superficially to the flexor retinaculum. It enters the hand via the ulnar canal (or Guyon’s canal). In the hand the nerve terminates by giving rise to superficial and deep branches.
Motor function
The ulnar nerve innervates muscles in the anterior compartment of the forearm, and in the hand.
In the anterior forearm, the muscular branch of the ulnar nerve supplies two muscles:
- Flexor carpi ulnaris – Flexes and adducts the hand at the wrist.
- Flexor digitorum profundus (medial half) – Flexes the fingers.
The remaining muscles in the anterior forearm are innervated by the median nerve.
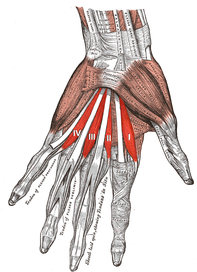
The majority of the intrinsic hand muscles are innervated by the deep branch of the ulnar nerve.
The hypothenar muscles (a group of muscles associated with the little finger) are innervated by the ulnar nerve. It also innervates some other muscles of the hand:
- Medial two lumbricals
- Adductor pollicis
- Interossei of the hand
- Palmaris brevis
The other muscles in the hand (such as the thenar eminence) are innervated by the median nerve.
Sensory function
There are three branches of the ulnar nerve that are responsible for its cutaneous innervation.
Two of these branches arise in the forearm, and travel into the hand:
- Palmar cutaneous branch: Innervates the skin of the medial half of the palm.
- Dorsal cutaneous branch: Innervates the skin of the medial one and a half fingers, and the associated dorsal hand area.
The last branch arises in the hand itself:
- Superficial branch – Innervates the palmar surface of the medial one and a half fingers.
Clinical relevance
Ulnar nerve entrapment is classified by location of entrapment. The ulnar nerve passes through several small spaces as it courses through the medial side of the upper extremity, and at these points the nerve is vulnerable to compression or entrapment. The nerve is particularly vulnerable to injury when there has been a disruption in the normal anatomy. The most common site of ulnar nerve entrapment is at the elbow, followed by the wrist.
Causes or structures which have been reported to cause ulnar nerve entrapment include:
- Problems originating at the neck: thoracic outlet syndrome, cervical spine pathology, compression by anterior scalene muscles
- Problems originating in the chest: compression by pectoralis minor muscles
- Brachial plexus abnormalities
- Elbow: fractures, growth plate injuries, cubital tunnel syndrome, flexorpronator aponeurosis, arcade of Struthers
- Forearm: tight flexor carpi ulnaris muscles
- Wrist: fractures, ulnar tunnel syndrome, hypothenar hammer syndrome
- Artery aneurysms or thrombosis
- Other: Infections, tumors, diabetes, hypothyroidism, rheumatism, and alcoholism
The most common location of ulnar nerve impingement at the elbow is within the cubital tunnel, and is known as cubital tunnel syndrome. The tunnel is formed by the medial epicondyle of the humerus, the olecranon process of the ulna and the tendinous arch joining the humeral and ulnar heads of the flexor carpi ulnaris muscle. While most cases of injury are minor and resolve spontaneously with time, chronic compression or repetitive trauma may cause more persistent problems. Commonly cited scenarios include:
- Sleeping with the arm folded behind neck, elbows bent.
- Pressing the elbows upon the arms of a chair while typing.
- Resting or bracing the elbow on the arm rest of a vehicle.
- Bench pressing.
- Intense exercising and strain involving the elbow.
- Guyon's canal syndrome
Ulnar nerve impingement along an anatomical space in the wrist called Guyon's canal is known as Guyon's canal syndrome, or ulnar tunnel syndrome. Recognized causes of ulnar nerve impingement at this location include local trauma, fractures, ganglion cysts, and classically avid cyclists who experience repetitive trauma against bicycle handlebars. This form of ulnar neuropathy comprises two work-related syndromes: so-called "hypothenar hammer syndrome," seen in workers who repetitively use a hammer, and "occupational neuritis" due to hard, repetitive compression against a desk surface.
Ulnar claw
An ulnar claw may follow an ulnar nerve lesion which results in the partial or complete denervation of the ulnar (medial) two lumbricals of the hand. Since the ulnar nerve also innervates the 3rd and 4th lumbricals, which flex the MCP joints, their denervation causes these joints to become extended by the now unopposed action of the long finger extensors (extensor digitorum and the extensor digiti minimi). The lumbricals and interossei also extend the interphalangeal (IP) joints of the fingers by insertion into the extensor hood; their paralysis results in weakened extension. The combination of hyperextension at the MCP and flexion at the IP joints gives the hand its claw like appearance.

Ulnar paradox
The ulnar nerve also innervates the ulnar (medial) half of the flexor digitorum profundus muscle (FDP). If the ulnar nerve lesion occurs more proximally (closer to the elbow), the flexor digitorum profundus muscle may also be denervated. As a result, flexion of the IP joints is weakened, which reduces the claw-like appearance of the hand. Instead, the fourth and fifth fingers are simply paralyzed in their fully extended position. This is called the "ulnar paradox" because one would normally expect a more proximal and thus debilitating injury to result in a more deformed appearance. As reinnervation occurs along the ulnar nerve after a high lesion, the deformity will first get worse (FDP reinnervated) as the patient recovers - hence the use of the term "paradox". A simple way to remember this is: 'the closer to the Paw, the worse the Claw'.



