Trigeminal nerve
The trigeminal nerve, CN V, is the fifth paired cranial nerve. It is also the largest cranial nerve. In this article, we shall look at the anatomical course of the nerve, and the motor, sensory and parasympathetic functions of its terminal branches.
The trigeminal nerve is associated with derivatives of the 1st pharyngeal arch.
Sensory: The three terminal branches of CN V innervate the skin, mucous membranes and sinuses of the face. Their distribution pattern is similar to the dermatome supply of spinal nerves (except there is little overlap in the supply of the divisions).
Motor: Only the mandibular branch of CN V has motor fibres. It innervates the muscles of mastication: medial pterygoid, lateral pterygoid, masseter and temporalis. The mandibular nerve also supplies other 1st pharyngeal arch derivatives: anterior belly of digastric, tensor veli palatini and tensor tympani.
Parasympathetic Supply: The post-ganglionic neurones of parasympathetic ganglia travel with branches of the trigeminal nerve. (But note that CN V is NOT part of the cranial outflow of PNS supply).
The trigeminal nerve originates from three sensory nuclei (mesencephalic, principal sensory, spinal nuclei of trigeminal nerve) and one motor nucleus(motor nucleus of the trigeminal nerve) extending from the midbrain to the medulla. A nucleus (pl. nuclei) is a collection of nerve cell bodies within the central nervous system.
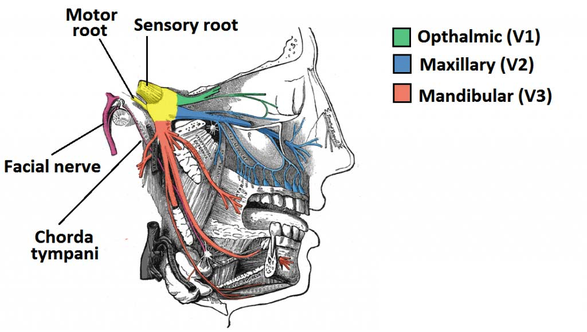
At the level of the pons, the sensory nuclei merge to form a sensory root. The motor nucleus continues to form a motor root. These roots are analogous to the dorsal and ventral roots of the spinal cord.In middle cranial fossa, the sensory root expands into the trigeminal ganglion. A ganglion (pl. ganglia) refers to a collection of the nerve cell bodies outside the central nervous system. The trigeminal ganglion is located lateral to the cavernous sinus, in a depression of the temporal bone. This depression is known as the trigeminal cave. The peripheral aspect of the trigeminal ganglion gives rise to 3 divisions: ophthalmic (V1), maxillary (V2) and mandibular (V3).
The motor root passes inferiorly to the sensory root, along the floor of the trigeminal cave. Its fibres are only distributed to the mandibular division.
The ophthalmic nerve and maxillary nerve travel lateral to the cavernous sinus exiting the cranium via the superior orbital fissure and foramen rotundum respectively. The mandibular nerve exits via the foramen ovale entering the infra-temporal fossa. (Note – be aware that while we talk about the nerves exiting the cranial cavity, the sensory components can also be said to be entering the cranial cavity, since they are afferent fibres).
Ophthalmic Nerve
Ophthalmic nerve gives rise to 3 terminal branches: frontal, lacrimal and nasociliary, which innervate the skin and mucous membrane of derivatives of the frontonasal prominence derivatives:
- Forehead and scalp
- Frontal and ethmoidal sinus
- Upper eyelid and its conjunctiva
- Cornea (see clinical relevance)
- Dorsum of the nose
- Parasympathetic Supply:
- Lacrimal gland: Post ganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve), travel with the zygomatic branch of V2 and then join the lacrimal branch of V1. The fibres supply parasympathetic innervation to the lacrimal gland.
Maxillary Nerve
Maxillary nerve gives rise to 14 terminal branches, which innervate the skin, mucous membranes and sinuses of derivatives of the maxillary prominence of the 1st pharyngeal arch:
- Lower eyelid and its conjunctiva
- Cheeks and maxillary sinus
- Nasal cavity and lateral nose
- Upper lip
- Upper molar, incisor and canine teeth and the associated gingiva
- Superior palate
Parasympathetic Supply:
- Lacrimal gland: Post ganglionic fibres from the pterygopalatine ganglion (derived from the facial nerve), travel with the zygomatic branch of V2 and then join the lacrimal branch of V1. The fibres supply parasympathetic innervation to the lacrimal gland.
- Nasal glands: Parasympathetic fibres are also carried to the mucous glands of the nasal mucosa. Post-ganglionic fibres travel with the nasopalatine and greater palatine nerves (branches of V2)
Mandibular Nerve
Mandibular nerve gives rise to four terminal branches in the infra-temporal fossa: buccal nerve, inferior alveolarnerve, auriculotemporal nerve and lingual nerve.
These branches innervate the skin, mucous membrane and striated muscle derivatives of the mandibular prominence of the 1st pharyngeal arch.
Sensory supply:
- Mucous membranes and floor of the oral cavity
- External ear
- Lower lip
- Chin
- Anterior 2/3 of the tongue (only general sensation; special taste sensation supplied by the chorda tympani, a branch of the facial nerve)
- Lower molar, incisor and canine teeth and the associated gingiva
Motor Supply:
- Muscles of mastication; medial pterygoid, lateral pterygoid, masseter, temporalis
- Anterior belly of the digastric muscle and the mylohyoid muscle (these are suprahyoid muscles)
- Tensor veli palatini
- Tensor tympani
Parasympathetic Supply:
- Submandibular and Sublingual glands: Post-ganglionic fibres from the submandibular ganglion (derived from the facial nerve), travel with the lingual nerve to innervate these glands.
- Parotid gland: Post-ganglionic fibres from the otic ganglion ganglion (derived from the glossopharyngeal nerve, CN IX), travel with the auriculotemporal branch of the V3 to innervate the parotid gland.
Clinical relevance
Peripheral lesions involving the sensory portion of the trigeminal at any point distal to the pontine exit can produce ipsilateral pain and/or varying degrees of anesthesia. The distribution of the lesion will, of course, determine the symptoms and findings.
Peripheral lesions: craniofacial trauma, basilar skull features, dental trauma, maxillary sinusitis, primary or metastatic tumors, aneurysm of the internal carotid artery, cavernous sinus thrombosis, stilbamidine, trichlorethylene, lupus, scleroderma, Sjøgren's syndrome, sarcoidosis, probably amyloidosis, and a fairly common idiopathic benign sensory neuropathy. Horner's syndrome can be produced by lesions of the nasociliary nerve as it runs with the ophthalmic division.
Lesions of the ganglion: herpes zoster infection, primary and metastatic tumors.
Trigeminal root lesions: adjacent tumors and vascular malformations, especially acoustic neurinoma and cholesteatomas. These lesions are prone to produce facial pain that is often misdiagnosed as tic douloureux or tooth pain.
Vascular lesions, tumors, and congenital malformations (syringobulbia and syringomyelia) are the common causes of central lesions. Lesions of the sensory cortex will produce a raised threshold (but not anesthesia) to pain and temperature on the opposite side of the face. Thalamic lesions can produce contralateral hypesthesia and hyperpathia of the face. Midpontine lesions, when unilateral, produce ipsilateral decrease in tactile sensation of the face due to involvement of the main sensory nucleus, and ipsilateral paralysis of the masticatory muscles when the motor nucleus is involved. Anesthesia or hypesthesia ipsilaterally is seen if the pontine lesion involves entering sensory root fibers carrying pain and temperature modalities. Below the pons, ipsilateral pain and temperature is lost if the spinal tract and nucleus are involved. When the ventral trigeminal tract carrying crossed pain–temperature fibers is involved, loss of these modalities occurs on the opposite side of the face.
Acoustic neuroma:
Both the motor and sensory divisions leave the brainstem at the side of the pons, accompanied by the facial nerve (VII) and also cranial nerve VIII or the acoustic nerve. These three nerves pass through the so-called “cerebellopontine angle” together. This is why an acoustic neuroma (CN VIII) can also affect the trigeminal nerve.
The trigeminal and facial nerves https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2848459/pdf/PE_7_1_25.pdf