Glossopharyngeal nerve
The glossopharyngeal nerve originates in the medulla oblongata of the brain. It emerges from the anterior aspect of the medulla, moving laterally in the posterior cranial fossa. The nerve leaves the cranium via the jugular foramen. At this point, the tympanic nerve arises. It has a mixed sensory and parasympathetic composition.
Immediately outside the jugular foramen lie two ganglia (collections of nerve cell bodies). They are known as the superiorand inferior (or petrous) ganglia – they contain the cell bodies of the sensory fibres in the glossopharyngeal nerve.
Now extracranial, the glossopharyngeal nerve descends down the neck, anterolateral to the internal carotid artery. At the inferior margin of the stylopharyngeus, several branches arise to provide motor innervation to the muscle. It also gives rise to the carotid sinus nerve, which provides sensation to the carotid sinus and body.
The nerve enters the pharynx by passing between the superior and middle pharyngeal constrictors. Within the pharynx, it terminates by dividing into several branches – lingual, tonsil and pharyngeal.
The glossopharyngeal nerve provides sensory innervation a variety of structures in the head and neck. The tympanic nerve arises as the nerve traverses the jugular foramen. It penetrates the temporal bone and enters the cavity of the middle ear. Here, it forms the tympanic plexus – a network of nerves that provide sensory innervation to the middle ear, internal surface of the tympanic membrane and Eustachian tube. At the level of the stylopharyngeus, the carotid sinus nerve arises. It descends down the neck to innervate both the carotid sinus and carotid body, which provide information about blood pressure and oxygen saturation respectively.
The glossopharyngeal nerve terminates by splitting into several sensory branches:
- Pharyngeal branch – combines with fibres of the vagus nerve to form the pharyngeal plexus. It innervates the mucosa of the oropharynx.
- Lingual branch – provides the posterior 1/3 of the tongue with general and taste sensation
- Tonsillar branch – forms a network of nerves, known as the tonsillar plexus, which innervates the palatine tonsils.
The glossopharyngeal nerve provides parasympathetic innervation to the parotid gland. These fibres originate in the inferior salivatory nucleus of CN IX. These fibres travel with the tympanic nerve to the middle ear. From the ear, the fibres continue as the lesser petrosal nerve, before synapsing at the otic ganglion. The fibres then hitchhike on the auriculotemporal nerve to the parotid gland, where they have a secretomotor effect.
Clinical relevance
Damage to the glossopharyngeal nerve can result in loss of taste sensation to the posterior one third of the tongue, and impaired swallowing.
Glossopharyngeal neuralgia is a rare condition characterized by paroxysms of pain in the sensory division of the cranial nerve IX. Although the pain of glossopharyngeal neuralgia is similar to that of trigeminal neuralgia, it occurs 100 times less frequently. Glossopharyngeal neuralgia occurs more commonly in patients older than 50 years. The pain is located in the tonsil, laryngeal region, and posterior tongue. The pain is unilateral in most patients, but can occur bilaterally 2% of the time. Rarely, the pain of glossopharyngeal neuralgia is associated with bradyarrhythmias; in some patients, it is associated with syncope. These cardiac symptoms are thought to be due to overflow of neural impulses from the glossopharyngeal nerve to the vagus nerve. Although rare, this unusual combination of pain and cardiac arrhythmia can be lethal.
The nuclei to cranial nerves IX and X lie in the medulla oblongata, and lesions within the brainstem can cause both upper and lower motor neuron signs and symptoms. Postpolio syndrome, syringomyelia, and Arnold-Chiari malformation can result in both laryngeal paralysis and dysphagia. Motor neuron diseases including primary lateral sclerosis, amyotrophic lateral sclerosis, progressive bulbar palsy, and progressive spinal muscular atrophy can also lead to laryngeal pathology.
Amyotrophic lateral sclerosis (ALS) is a devastating motor neuron disease defined by degeneration of upper and lower motor neurons. Thirty percent of patients have bulbar symptoms at the time of disease onset, and nearly all patients manifest bulbar involvement at the late stages of the disease.
Extrapyramidal contributions to cranial nerves IX and X are poorly understood, but can be significant causes of laryngeal and pharyngeal dysfunction. Movement disorders of the larynx include Parkinson’s, essential tremor, and spasmodic dysphonia. They are defined by inadequate motor control of the laryngeal musculature, resulting in irregular muscle tension, spasmodic contractions, or tremor. Patients experience irregular vocal production including strained voice, tremor, or pitch variability.
The glossopharyngeal and vagus nerves pass through the cerebellopontine angle (CPA) before exiting the skull. Mass lesions within the CPA may cause lower cranial nerve involvement. Vestibular schwannomas account for greater than 90% of all CPA tumors, and usually present with sensorineural hearing loss and disequilibrium.27 While some patients present with facial nerve weakness due to involvement of cranial nerve VII, involvement of the lower cranial nerves is exceedingly rare.
The glossopharyngeal, vagus, and accessory nerves exit the skull base together through the jugular foramen. Infection such as skull base osteomylitis, skull base fractures, or neoplasms may affect the three nerves in concert, resulting in ipsilateral vocal fold, palate, and shoulder weakness. In addition to the above symptoms, lesions within the retropharyngeal space may also involve the hypoglossal nerve and the ascending sympathetic chain, resulting in tongue weakness and Horner’s syndrome respectively.
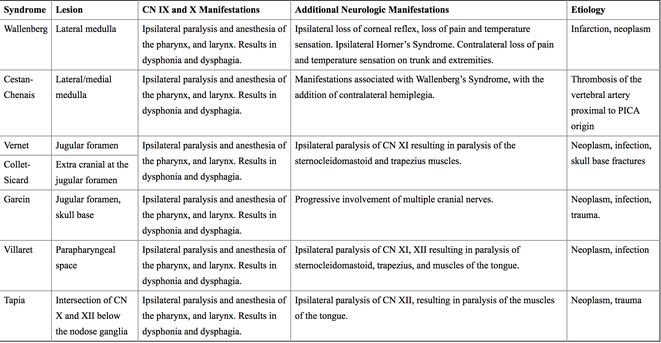
See table for other lesion sites in CN IX (and X) dysfunction.