Median nerve
The median nerve is derived from the medial and lateral cords of the brachial plexus. It contains fibres from all five roots (C5-T1).
After originating from the brachial plexus in the axilla, the median nerve descends down the arm, initially lateral to the brachial artery. Halfway down the arm, the nerve crosses over the brachial artery, and becomes situated medially. The median nerve enters the anterior compartment of the forearm via the cubital fossa.
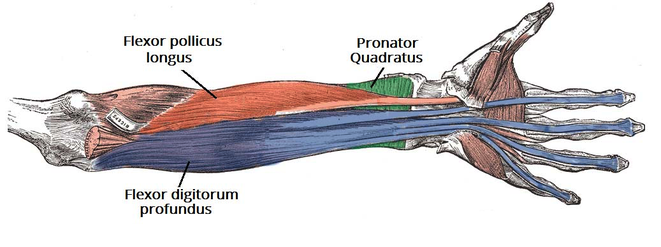
In the forearm, the nerve travels between the flexor digitorum profundus and flexor digitorum superficialis muscles. The median nerve gives rise to two major branches in the forearm:
- Anterior interosseous nerve – Supplies the deep muscles in the anterior forearm.
- Palmar cutaneous nerve – Innervates the skin of the lateral palm.
The median nerve enters the hand via the carpal tunnel, where it terminates by dividing into two branches:
- Recurrent branch – Innervates the thenar muscles.
- Palmar digital branch – Innervates the palmar surface and fingertips of the lateral three and half digits. Also innervates the lateral two lumbrical muscles.
Motor function
The median nerve innervates the majority of the muscles in the anterior forearm, and some intrinsic hand muscles.
The anterior forearm
In the forearm, the median nerve directly innervates muscles in the superficial and intermediate layers:
- Superficial layer: Pronator teres, flexor carpi radialis and palmaris longus.
- Intermediate layer: Flexor digitorum superficialis.
The median nerve also gives rise to the anterior interosseous nerve, which supplies the deep flexors:
- Deep layer: Flexor pollicis longus, pronator quadratus, and the lateral half of the flexor digitorum profundus (the medial half of the muscle is innervated by the ulnar nerve).
In general, these muscles perform pronation of the forearm, flexion of the wrist and flexion of the digits of the hand.
The hand
The median nerve innervates some of the muscles in the hand via two branches. The recurrent branch of the median nerve innervates the thenar muscles – muscles associated with movements of the thumb. The palmar digital branch innervates the lateral two lumbricals – these muscles perform flexion at the metacarpophalangeal joints of the index and middle fingers
The remaining muscles in the anterior forearm and hand are innervated by the ulnar nerve.
Sensory function
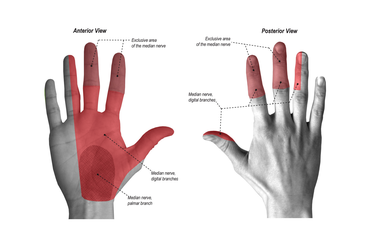
The median nerve is responsible for the cutaneous innervation of part of the hand. This is achieved via two branches:
-Palmar cutaneous branch – Arises in the forearm and travels into the hand. It innervates the lateral aspect of the palm. This nerve does not pass through the carpal tunnel, and is spared in carpal tunnel syndrome.
-Palmar digital cutaneous branch – Arises in the hand. Innervates the palmar surface and fingertips of the lateral three and half digits.
Clinical relevance
Entrapment syndromes of the median nerve represent the median nerve being compressed at a number of distinct sites leading to a number of distinct clinical syndromes.
Entrapment is but one of the gamut of pathologies causing neuropathy, albeit one of the more common etiologies. Entrapment syndromes as a rule affect nerves at defined anatomical locations, facilitating a more focused search for causative lesions. The three most common median nerve entrapment syndromes are:
- pronator teres syndrome (PTS)
- anterior interosseous nerve syndrome (AINS) (aka Kiloh-Nevin syndrome)
- carpal tunnel syndrome (CTS)
Pronator teres syndrome
PTS can present with:
- volar pain of the proximal lower arm
- paresthesia of the volar forearm and the radial three digits and radial aspect of the fourth digit
- weakness, on the other hand, is variable, often with unspecified grip clumsiness
- the proximal volar forearm is painful to palpation, and Tinel’s sign can be elicited on palpation of the pronator teres muscle
Symptoms provoked by examination maneuvers, such as during resisted forearm pronation (suggesting median nerve compression by pronator teres muscle), or resisted elbow flexion and forearm supination (indicating median nerve compression by biceps aponeurosis / lacertus fibrosus) can help pinpoint the site of compression.
Clinical presentation can harbor some pitfalls. Sensory and pain symptoms of PTS and carpal tunnel syndrome can overlap: distinguish the two by looking for numbness of the forearm, which does not occur in CTS, and asking about nocturnal exacerbation, which would atypical in PTS.
In complete PTS, affected muscles are the pronator teres (PT), flexor carpi radialis (FCR), palmaris longus (PL), flexor digitorum superficialis (FDS), along with muscles innervated by the anterior interosseous nerve.
Anterior interosseous nerve syndrome
AINS is a rare entrapment syndrome, with comparatively little robust epidemiological data. AINS is said to account for less than 1% of neuropathies of the upper limb.
AINS is a pure motor neuropathy, as the anterior interosseous nerve contains no sensory fibres; dull forearm pain is however sometimes mentioned by patients.
Typically, patients fail to make an “O.K.”-sign, as flexion of the interphalangeal joint of the thumb and the distal interphalangeal joint of the index finger is impaired. Another sensitive test is the pinch test: a patient with AINS will also not be able to pinch a sheet of paper between his thumb and index finger, instead clamping the sheet between his extended thumb and index fingers, akin to a tong rather than a clamp. Weakness of the pronator quadratus muscle manifests itself in pronation weakness with a flexed elbow.
AINS can be confounded by the Martin-Gruber anastomosis, present in up to 25% of the population: in these cases, the anterior interosseous nerve gives off branches to the ulnar nerve, creating atypical motor innervation patterns of the forearm and hand and thus effacing the typical clinical symptoms.
The aetiology is highly debated. Two common causes of AINS are compression neuropathy and brachial plexus neuritis.
In complete AINS, the flexor pollicis longus (FPL), the radial part (2nd and 3rd digit) of the flexor digitorum profundus (FDP) and pronator quadratus (PQ) are affected.
Carpal tunnel syndrome
CTS results from compression of the median nerve within the carpal tunnel. It is a cause of significant disability and is one of three common median nerve entrapment syndromes, the other two being anterior interosseous nerve syndrome and pronator teres syndrome.
The prevalence of carpal tunnel syndrome is estimated to be 2.7-5.8% of the general adult population, with a lifetime incidence of 10-15%, depending on occupational risk.
Carpal tunnel syndrome usually occurs between ages 36 and 60 and is more common in women, with a female-to-male ratio of 2-5:1.
Carpal tunnel syndrome is primarily defined by pain and sensory symptoms:
- brachialgia paraesthetica nocturna, or nocturnal ascending pain emanating from the wrist, is typical
sensory symptoms affect the first three digits and, depending on innervation patterns, the radial aspect of the fourth digit
- positive Tinel test: paraesthesias elicited by tapping the median nerve at the wrist
- positive Phalen test: paraesthe.sias caused by wrist flexion over 30-60°
- Hand weakness, as a rule, is a late and often functionally irrelevant symptom.
The dominant hand is affected more frequently, and bilateral involvement has been reported to occur in ~30% (range 8-50%) of cases.
Clinical signs
A lesion to the upper arm area, just proximal to where motor branches of forearm flexors originate, is diagnosed if the patient is unable to make a fist. More specifically, the patient's index and middle finger cannot flex at the MCP joint, while the thumb usually is unable to oppose. This is known as hand of benediction or Pope’s blessing hand. Another test is the bottle sign—the patient is unable to close all their fingers around a cylindrical object.
In "Ape hand deformity" (simian hand), the thenar muscles become paralyzed due to impingement and are subsequently flattened. This hand deformity is not by itself an individual diagnosis; it is seen only after the thenar muscles have atrophied. While the adductor pollicis remains intact, the flattening of the muscles causes the thumb to become adducted and laterally rotated. The opponens polliciscauses the thumb to flex and rotate medially, leaving the thumb unable to oppose. Carpal tunnel syndrome can result in thenar muscle paralysis which can then lead to ape hand deformity if left untreate. Ape hand deformity can also be seen in the hand of benediction deformity.