Fibromuscular dysplasia
FMD is a nonatherosclerotic, noninflammatory vascular disease that may result in arterial stenosis, occlusion, aneurysm, or dissection. FMD has been found in nearly every arterial bed in the body although the most common arteries affected are the renal and carotid arteries.
FMD is frequently asymptomatic. Symptomatic patients commonly present with:
- hypertension or less commonly renal impairment due to renal artery stenosis
- CNS symptoms (e.g. headache, neck pain, pulsatile tinnitus, Horner syndrome) from transient ischaemic attack, stroke, dissection, due to carotid and vertebral artery involvement
- angina, myocardial infarction or sudden cardiac death due to coronary artery involvement
- symptoms of mesenteric ischaemia (mesenteric infarction is rare due to formation of collateral supply)
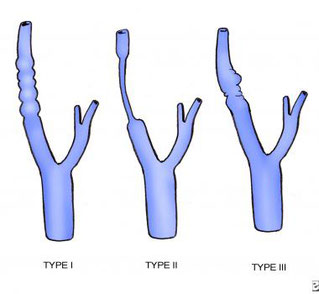
There are various types of FMD, with multi-focal fibroplasia being the most common. Further, less common, forms of the disease include focal (previously known as intimal) and adventitial fibroplasia. FMD predominantly affects middle-aged women, but has been found in men and people of all ages. Pediatric cases of FMD are vastly different from that of the adult population, and poorly studied. The prevalence of FMD is not known and, although the disease was initially thought to be rare, recent studies have suggested that it may be underdiagnosed.
Arterial imaging with CT angiography, MR angiography and digital subtraction angiography (DSA) may be used to visualise the lesions in FMD. Selective DSA is the gold standard because it allows visualisation of small or peripheral lesions. The characteristic finding, particularly in more common intimal subtype, is alternating stenoses and dilatations, causing a string of beads-appearance. Less commonly in intimal and adventitial type, there is focal concentric, long-segment tubular stenosis or diverticular outpouching present. Cross-sectional imaging (CT and MRI) allows assessment of end-organ ischaemic damage.
Fibromuscular dysplasia cannot be cured. Treatment of the disease consists of risk management and symptom relieve. Angioplasty is recommended for patients with renal artery FMD who have uncontrollable blood pressure, intolerance of medications, or declining kidney function. For some patients with newly diagnosed high blood pressure caused by renal artery FMD, angioplasty may also be recommended. Unlike patients with renal artery disease caused by atherosclerosis (or plaque), for patients with renal FMD, balloon angioplasty is generally performed without placement of a metallic stent. Angioplasty is most likely to be effective at controlling or curing high blood pressure in patients who do not have other risk factors associated with high blood pressure (such as obesity or diabetes mellitus) and in those who have had high blood pressure for a short period of time (<5 years).
In some cases, angioplasty may also be performed in patients with carotid or vertebral artery FMD who have severe neurological symptoms. For symptomatic patients with carotid or vertebral artery FMD who have suffered a dissection, angioplasty with placement of a metallic stent may be performed. In less common cases, patients with FMD in the arteries of the arms, legs, or intestines may also undergo an angioplasty procedure to relieve symptoms caused by the arterial narrowing.
The vascular subtype of Ehlers-Danlos Syndrome (type IV) has been associated with multi-focal FMD. This syndrome should be suspected in patients with multiple aneurysms and/or tears (dissections) in arteries in addition to the typical angiographic findings of FMD. There have been isolated reports of FMD associated with other disorders, including Alport syndrome, pheochromocytoma, Marfan syndrome, Moyamoya disease, and Takayasu's arteritis.