Axillary nerve
The axillary nerve is formed within the axilla region. It is a direct continuation of the posterior cord of the brachial plexus, and therefore contains fibres from the C5 and C6 nerve roots.
Immediately after its formation, the axillary nerve lies posteriorly to the axillary artery and anteriorly to the subscapularis muscle. It descends to the inferior border of the subscapularis muscle, and then exits the axilla posteriorly via the quadrangular space. It is accompanied by the posterior circumflex humeral artery.
In the posterior scapular region, the axillary nerve terminates by dividing into two branches:
- Posterior terminal branch – Provides motor innervation to the teres minor muscle, and innervates the skin over the inferior part of the deltoid.
- Anterior terminal branch – Provides motor innervation to the deltoid muscle
The axillary nerve also provides articular branches to the shoulder joint itself.
Motor function
The axillary nerve innervates the teres minor and the deltoid muscles.
The teres minor is part of the rotator cuff muscles of the shoulder. This set of muscles acts to stabilise the glenohumeral joint. Acting individually, the teres minor externally rotates the upper limb. The muscle is innervated the posterior terminal branch of the axillary nerve.
The deltoid is situated at the superior aspect of the shoulder. It performs abduction of the upper limb at the glenohumeral joint. The muscle is innervated by the anterior terminal branch of the axillary nerve.
Sensory function
The sensory component of the axillary nerve is delivered via its posterior terminal branch.
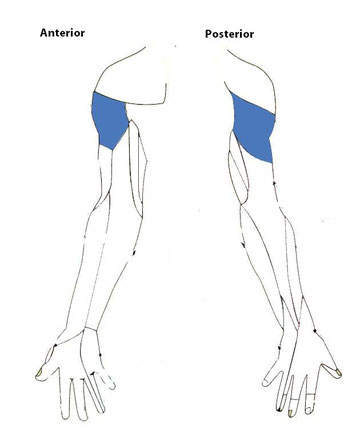
After the posterior terminal branch of the axillary nerve has innervated the teres minor, it continues as the upper lateral cutaneous nerve of the arm. This nerve innervates the skin over the inferior portion of the deltoid (known as the ‘regimental badge area’).
Clinical relevance
In a patient with axillary nerve damage, sensation at the regimental badge area may be impaired or absent. The patient may also report paraesthesia (pins and needles) in the distribution of the axillary nerve.
Patients may have paralysis of the deltoid and teres minor muscles, rendering them unable to abduct the affected limb.
In long standing cases, the paralysed deltoid muscle rapidly atrophies, and the greater tuberosity can be palpated in that area.