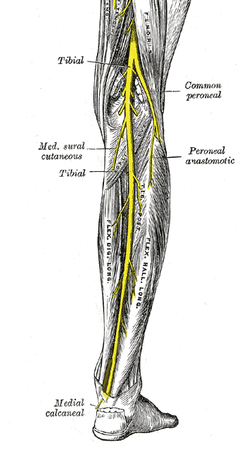
Tibial nerve
The tibial nerve is a branch of the sciatic nerve, and arises at the apex of the popliteal fossa. It travels through the popliteal fossa, giving off branches to muscles in the superficial posterior compartment of the leg. Here, the tibial nerve also gives rise to branches that contribute towards the sural nerve, which innervates the posterolateral aspect of the leg. The tibial nerve continues its course down the leg, posterior to the tibia. During its descent, it supplies the deep muscles of the posterior leg.
At the foot, the nerve passes posteriorly and inferiorly to the medial malleolus, through a structure known as the tarsal tunnel. This tunnel is covered superiorly by the flexor retinaculum. Within this tunnel, branches arise from the tibial nerve to supply cutaneous innervation to the heel.
Immediately distal to the tarsal tunnel, the tibial nerve terminates by dividing into sensory branches, which innervate the sole of the foot.
Click image to enlarge
Motor function
The tibial nerve innervates all the muscles in the posterior compartment of the leg. They are divided into a deep and superficial compartment:
Deep:
- Popliteus – Laterally rotates the femur on the tibia to unlock the knee.
- Flexor Hallucis Longus – Flexes the big toe and plantar flexes the ankle.
- Flexor digitorum Longus – Flexes the other digits and plantar flexes the ankle.
- Tibialis Posterior – Inverts the foot and plantar flexes the ankle.
Superficial:
- Plantaris – Plantar flexes the ankle.
- Soleus – Plantar flexes the ankle.
- Gastrocnemius – Plantar flexes the ankle and flexes the knee.
Sensory function
In the popliteal fossa, the tibial nerve gives off cutaneous branches. These combine with branches from the common fibular nerve to form the sural nerve. This sensory nerve innervates the skin of the posterolateral side of the leg and the lateral side of the foot.
The tibial nerve also supplies all the sole of the foot via three branches:
- Medial calcaneal branches: These arise within the tarsal tunnel, and innervate the skin over the heel.
- Medial Plantar Nerve: Innervates the plantar surface of the medial three and a half digits, and the associated sole area.
- Lateral Plantar Nerve: Innervates the plantar surface of the lateral one and a half digits, and the associated sole area.
Clinical relevance
Damage to the tibial nerve is rare, and is often a result of direct trauma, entrapment through narrow space or compression for long period of time. Damage results in loss of plantar flexion, loss of flexion of toes and weakened inversion (The tibialis anterior can still invert the foot).
The tibial nerve is not part of the conventional popliteal artery entrapment syndrome. Occasionally the tibial nerve may be compressed in the popliteal fossa. Nerve compression by popliteal cysts and by hemorrhage associated with popliteal muscle rupture has been reported.
Tarsal tunnel syndrome
A condition that is caused by compression of the tibial nerve or its associated branches as the nerve passes underneath the flexor retinaculum at the level of the ankle or distally. It is analogous to carpal tunnel syndrome of the wrist.
Tarsal tunnel syndrome is a multifaceted compression neuropathy that typically manifests with pain and paresthesias that radiate from the medial ankle distally and, occasionally, proximally. These findings may have a variety of causes, which can be categorized as extrinsic, intrinsic, or tensioning factors in the development of signs and symptoms of tarsal tunnel syndrome.
Extrinsic causes may contribute to the development of tarsal tunnel syndrome. Examples include external trauma due to crush injury, stretch injury, fractures, dislocations of the ankle and hindfoot, and severe ankle sprains.
Local causes may be intrinsic causes of the neuropathy. Examples include space-occupying masses, localized tumors, bony prominences, and a venous plexus within the tarsal canal.
Nerve tension caused by a valgus foot can cause symptoms that are identical to those of a circumferential nerve compression.
Symptoms of tarsal tunnel syndrome vary from individual to individual, but clinical findings generally include the following:
- Sensory disturbance that varies from sharp pain to loss of sensation
- Motor disturbance with resultant atrophy of intrinsic musculature
- Gait abnormality (eg, overpronation and a limp due to pain with weightbearing)
A hindfoot valgus deformity may potentiate the symptoms of tarsal tunnel syndrome because the deformity may increase tension due to an increase in eversion and dorsiflexion.