Vagus nerve
The vagus nerve has the longest course of all the cranial nerves, extending from the head to the abdomen. Its name is derived from the Latin ‘vagary’ – meaning wandering. It is sometimes referred to as the wandering nerve.
The vagus nerve originates from the medulla of the brainstem. It exits the cranium via the jugular foramen, with the glossopharyngeal and accessory nerves (CN IX and XI respectively).
Within the cranium, the auricular branch arises. This supplies sensation to the posterior part of the external auditory and canal external ear.
In the neck, the vagus nerve passes into the carotid sheath, travelling inferiorly with the internal jugular vein and common carotid artery. At the base of the neck, the right and left nerves have differing pathways:
- The right vagus nerve passes anterior to the subclavian artery and posterior to the sternoclavicular joint, entering the thorax.
- The left vagus nerve passes inferiorly between the left common carotid and left subclavian arteries, posterior to the sternoclavicular joint, entering the thorax.
Several branches arise in the neck:
- Pharyngeal branches – Provides motor innervation to the majority of the muscles of the pharynx and soft palate.
- Superior laryngeal nerve – Splits into internal and external branches. The external laryngeal nerve innervates the cricothyroid muscle of the larynx. The internal laryngeal provides sensory innervation to the laryngopharynx and superior part of the larynx.
- Recurrent laryngeal nerve (right side only) – Hooks underneath the right subclavian artery, then ascends towards to the larynx. It innervates the majority of the intrinsic muscles of the larynx.
In the thorax, the right vagus nerve forms the posterior vagal trunk, and the left forms the anterior vagal trunk. Branches from the vagal trunks contribute to the formation of the oesophageal plexus, which innervates the smooth muscle of the oesophagus.
Two other branches arise in the thorax:
- Left recurrent laryngeal nerve – it hooks under the arch of the aorta, ascending to innervate the majority of the intrinsic muscles of the larynx.
- Cardiac branches – these innervate regulate heart rate and provide visceral sensation to the organ.
The vagal trunks enter the abdomen via the oesophageal hiatus, an opening in the diaphragm.
In the abdomen, the vagal trunks terminate by dividing into branches that supply the oesophagus, stomach and the small and large bowel (up to the splenic flexure).
There are somatic and visceral components to the sensory function of the vagus nerve.
Somatic refers to sensation from the skin and muscles. This is provided by the auricular nerve, which innervates the skin of the posterior part of the external auditory canal and external ear.
Viscera sensation is that from the organs of the body. The vagus nerve innervates:
- Laryngopharynx – via the internal laryngeal nerve.
- Superior aspect of larynx (above vocal folds) – via the internal laryngeal nerve.
- Heart – via cardiac branches of the vagus nerve.
- Gastro-intestinal tract (up to the splenic flexure) – via the terminal branches of the vagus nerve.
The vagus nerve has a minor role in taste sensation. It carries afferent fibres from the root of the tongue and epiglottis.
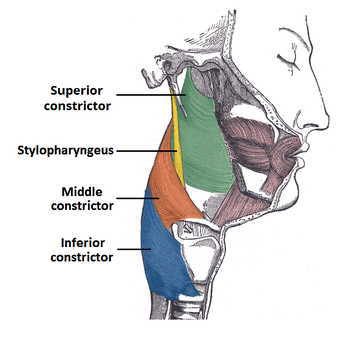
Most of the muscles of the pharynx are innervated by the pharyngeal branches of the vagus nerve:
- Superior, middle and inferior pharyngeal constrictor muscles
- Palatopharyngeus
- Salpingopharyngeus
Innervation to the intrinsic muscles of the larynx is achieved via the recurrent laryngeal nerve and external branch of the superior laryngeal nerve.
Recurrent laryngeal nerve:
- Thyro-arytenoid
- Posterior crico-arytenoid
- Lateral crico-arytenoid
- Transverse and oblique arytenoids
- Vocalis
- External laryngeal nerve:
- Cricothyroid
In the thorax and abdomen, the vagus nerve is the main parasympathetic outflow to the heart and gastro-intestinal organs. Cardiac branches arise in the thorax, conveying parasympathetic innervation to the sino-atrial and atrio-ventricular nodes of the heart. These branches stimulate a reduction in the resting heart rate. They are constantly active, producing a rhythm of 60 – 80 beats per minute. If the vagus nerve was lesioned, the resting heart rate would be around 100 beats per minute.
The vagus nerve provides parasympathetic innervation to the majority of the abdominal organs. It sends branches to the oesophagus, stomach and most of the intestinal tract – up to the splenic flexure of the large colon. The function of the vagus nerve is to stimulate smooth muscle contraction and glandular secretions in these organs.
Clinical relevance
The vagus nerve can be affected by pathology from its origin to anywhere along its course.
As the vagus nerve is mostly parasympathetic, sensory clinical features can be subtle or absent, especially when affected below the origin of the recurrent laryngeal nerves.
Features include:
- deviation of the uvula away from affected side
- ipsilateral loss of pharyngeal reflex
- ipsilateral vocal cord paralysis
Supranuclear lesions affecting the vagus often involve other cranial nerves as well, including cranial nerves IX, XI and XII. Unilateral lesions typically reveal little or no deficit due to the bilateral input to the nucleus ambiguus from the corticobulbar regions. Pseudobulbar palsy can occur when there are bilateral corticobulbar lesions.
Brainstem lesions that may affect the vagus include:
- brainstem neoplasms
- demyelinating/inflammatory disease
- vascular disease
- syringobulbia
- Avellis syndrome
Jugular foramen lesions:
- jugular foramen syndrome (Vernet syndrome)
- fractures involving the base of the skull
- neoplasms involving the base of the skull
- neoplasms within the jugular foramen such as glomus jugulare, meningioma, and schwannoma
Extracranial lesions:
- vagus nerve mononeuritis
- trauma
- infiltration by tumour
primary tumours of the vagus nerve:
- vagal schwannoma
- vagal neurofibroma
The recurrent laryngeal nerves travel through the mediastinum before entering the larynx, and they are susceptible to injury throughout their course. The left recurrent laryngeal nerve is more often injured than the right, as it has a longer course through the mediastinum back into the larynx. Specific etiologies in the mediastinum include lung or thoracic malignancies and metastatic lesions. Cardiovocal syndrome, also known as Ortner’s syndrome, is the association of hoarseness due to a left recurrent laryngeal nerve palsy caused by cardiovascular pathology. First described in patients with left atrial enlargement secondary to mitral valve stenosis, it is now recognized that a host of cardiovascular pathologies may cause impingement of the left recurrent laryngeal nerve between the aorta and pulmonary artery