Glioblastoma multiforme
Glioblastoma multiforme (GBM) or glioblastoma, is the most common primary intracranial neoplasm. It accounts for 15% of all intracranial neoplasms and approximately half of all astrocytomas.
GBMs are high grade (WHO grade IV) astrocytomas with a poor prognosis. They tend to spread along the white matter tracts and corpus callosum, occasionally involving the contralateral hemisphere. Lesions can be solitary (with or without satellite lesions) or multifocal. Glioblastomas can be primary tumors (de novo, 90%) or de-differentiate from a lower grade tumor (10%).
Epidemiology
Glioblastomas occur at any age, but usually occur after the age of 40 years with a peak incidence between 65 and 75 years of age. There is a slight male predilection with a 3:2 ratio. Caucasians are affected more frequently than other ethnicities: Europe and North America 3-4 per 100,000 whereas Asia 0.59 per 100,000.
The vast majority of glioblastomas are sporadic. Rarely they are related to prior radiation exposure (radiation-induced GBM). They can also occur as part of rare inherited tumour syndromes, such as p53 mutation related syndromes such as neurofibromatosis type1 (NF1) and Li-Fraumeni syndrome. Other syndromes in which GBMs are encountered include Turcot syndrome, Ollier disease and Maffucci syndrome.
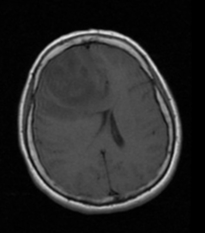
MRI features
T1: T1 weighted imaging shows a hypo- to isointense mass within white matter, sometimes with a central heterogeneous signal (necrosis, intratumoral haemorrhage)
T1 C+ (Gd): Contrast-enhancement is variable but is almost always present, typically peripheral and irregular with nodular components and usually surrounds necrosis
T2/FLAIR: T2 shows a hyperintense signal surrounded by vasogenic oedema. Ocassionaly flow voids are seen.
GE/SWI: Susceptibility artefact on T2* from blood products may be seen.
DWI/ADC: An elevated signal on DWI is common in the solid/enhancing component.
Diffusion restriction is typically intermediate similar to normal white matter, but significantly elevated compared to surrounding vasogenic oedema.
MR perfusion: Perfusion rates are elevated compared to lower grade tumours and normal brain